Critical Steps in Heart Attack Treatment
When someone has a heart attack, medically known as an acute myocardial infarction (AMI), the speed of treatment is crucial. The term “door-to-balloon time” (D2B) refers to the interval from when a patient arrives at the hospital to receiving treatment to open the blocked artery. The faster this treatment happens, the better the chances of survival and recovery. This period can be broken down into six main stages, each critical in the overall treatment process. Each stage is ideally targeted to be completed within a 10-minute interval.

- Door to ECG Time: This is when the patient arrives at the hospital and receives an electrocardiogram (ECG). The ECG is a quick, painless test recording the heart’s electrical activity. It is essential for diagnosing a heart attack and determining its severity. Rapid ECG acquisition is crucial because it sets the stage for all subsequent actions.
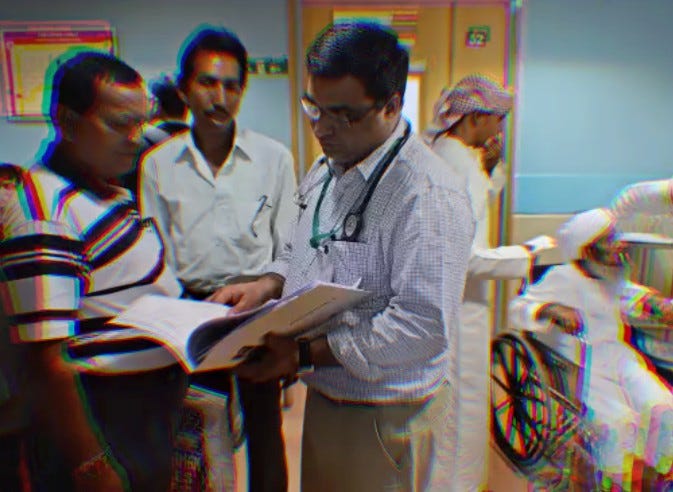
- Decision Time for PCI by the CCU Team: After the ECG results are available, the Coronary Care Unit (CCU) team or the emergency department staff must quickly interpret the results and decide to proceed with Primary Percutaneous Coronary Intervention (PPCI). This decision involves evaluating the patient’s clinical condition, confirming the STEMI diagnosis, and determining the urgency of intervention. Quick and accurate decision-making at this stage is vital to minimize delays.
- Time for Consent for PPCI: Once the decision for PPCI is made, obtaining informed consent from the patient or their family is necessary. This involves explaining the procedure and its risks, benefits, and alternatives to the patient or their family members. The consent process should be handled efficiently to avoid unnecessary delays while ensuring the patient and their family fully understand what will happen.
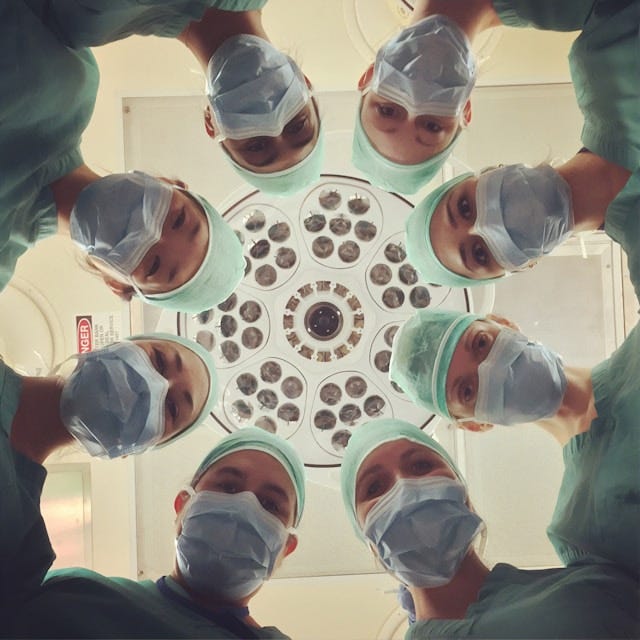
- Time for STEMI Team Activation: The STEMI (ST-Elevation Myocardial Infarction) team, which includes interventional cardiologists, nurses, and other support staff, must be activated promptly. This step involves notifying the catheterization lab team to prepare for the procedure and ensuring all necessary personnel are available and ready. Effective communication and coordination are crucial to minimizing delays at this stage.
- Financial Process Time: In some healthcare systems, financial clearance or administrative processes may need to be completed before the procedure. While this should not delay emergency care, it may affect the overall D2B time in certain institutions. It is crucial to streamlining financial processes and ensuring they do not hinder emergency treatment.
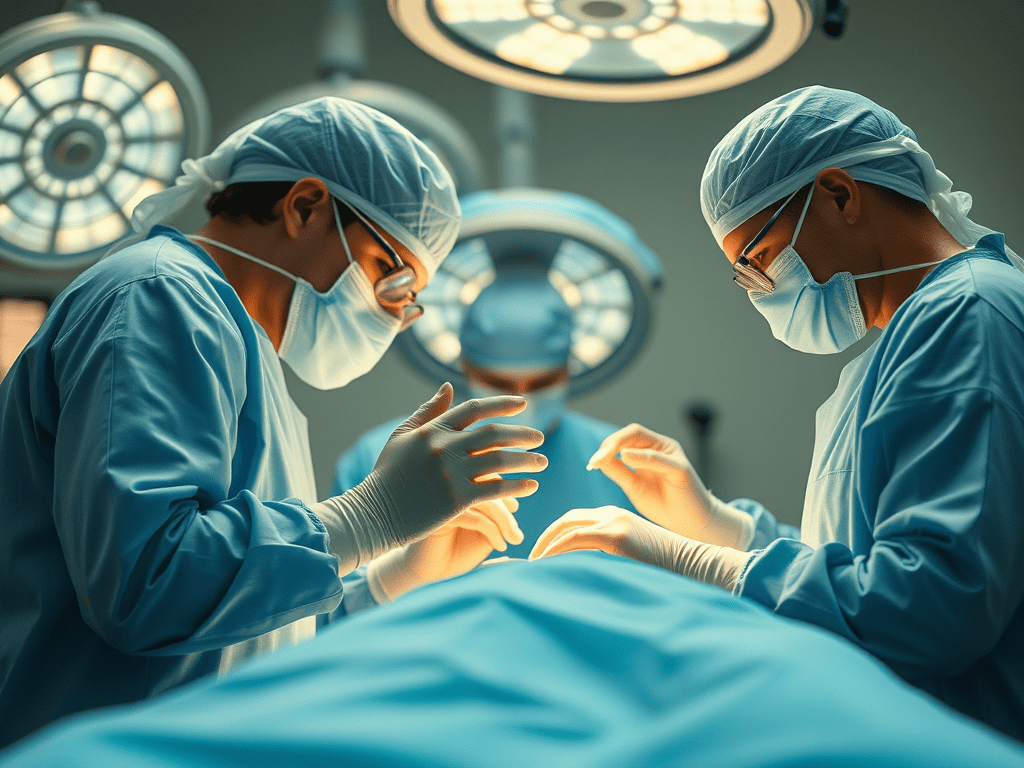
- Sheath to Balloon Time: When the balloon catheter is first inflated in the blocked coronary artery, the patient is wheeled into the catheterization lab. This stage includes prepping the patient, inserting the vascular sheath, navigating the coronary anatomy, and deploying the balloon to open the blocked artery. The cath lab team’s efficient operation is essential to minimize time at this stage.
Challenges in India
In India, various factors contribute to delays in each of these stages, significantly impacting patient outcomes. Understanding these challenges is crucial for developing effective strategies to improve D2B times and patient outcomes.
Patient and Attendant Awareness
A critical issue is the lack of awareness among patients and their attendants about the urgency of heart attack treatment. Many patients delay seeking medical help because they do not recognize the symptoms of a heart attack or underestimate the severity of their condition. Symptoms like chest pain, shortness of breath, and discomfort in the upper body should not be ignored. Additionally, there is often a reluctance to trust healthcare providers’ recommendations. This mistrust can stem from past negative experiences, fear of medical procedures, or misinformation about the benefits and risks involved. Public education campaigns are essential to raise awareness about the symptoms of heart attacks and the importance of immediate medical attention.
Decision-Making and Negligence
Another significant problem is hesitation in making swift decisions about treatment. Some patients and families opt for a second opinion, leading to critical time loss. This indecisiveness can stem from a need for more understanding of the critical nature of timely intervention in a heart attack. Educating patients and their families about the importance of rapid treatment and the consequences of delays is vital. Healthcare providers should communicate clearly and compassionately to build trust and facilitate quick decision-making.
Economic Burden
The cost of cardiac care is a substantial barrier, particularly in private hospitals. The financial burden can deter patients from opting for timely and necessary interventions. While costs are lower in government hospitals, there might be delays due to administrative processes or a lack of resources. Financial barriers can lead to dangerous delays in treatment. Implementing financial assistance programs and insurance schemes can help alleviate this burden and ensure that cost does not prevent patients from receiving timely care.
Urban and Rural Disparities
In urban areas, traffic congestion can significantly delay a patient’s arrival at the hospital, even if the hospital is nearby. The heavy traffic in cities like Mumbai, Delhi, and Bangalore can turn a short drive into a lengthy ordeal, costing precious time. In contrast, rural areas face the challenge of limited access to tertiary healthcare facilities. Patients often need to travel long distances to reach a hospital capable of performing PPCI, which can lead to critical delays. Improving transportation infrastructure and increasing the number of tertiary care centres in rural areas can help reduce these delays.

Mortality and Complications
Delays in D2B time are directly linked to increased mortality and complications. Studies have shown that every 30-minute delay in treatment increases the risk of mortality. This risk is heightened in India, where D2B times are often prolonged due to the abovementioned issues. Complications such as heart failure, arrhythmias, and recurrent myocardial infarctions are more likely when treatment is delayed. Reducing delays at each stage of the D2B process can significantly improve patient outcomes and reduce the risk of long-term complications.
Opportunities for Improvement
To address these challenges, several strategies can be implemented:
- Public Awareness Campaigns: Educating the public about the signs of a heart attack and the importance of seeking immediate medical attention can help reduce delays. Campaigns should emphasize that prompt treatment can save lives and improve outcomes. Using various media platforms, including social media, television, and community outreach programs, can effectively spread awareness.
- Streamlining Hospital Processes: Hospitals can improve their internal processes to reduce time at each stage. This includes faster ECG acquisition, quicker decision-making protocols, and reduced administrative burdens. Implementing standardized protocols and ensuring that all staff are trained in these protocols can help streamline the process.
- Financial Assistance Programs: Implementing financial aid and insurance schemes can alleviate the economic burden on patients, ensuring they do not delay treatment due to cost concerns. Government and private partnerships can be explored to provide comprehensive coverage for heart attack treatment.
- Building Trust in Healthcare: Trust between healthcare providers and patients is crucial. Transparent communication and patient education can help patients gain confidence. Healthcare providers should take the time to explain the procedures, address concerns, and reassure patients and their families.
- Improving Infrastructure: Improving road infrastructure in urban areas to reduce traffic congestion and increasing the number of tertiary care centres in rural areas can reduce delays. Investments in healthcare infrastructure, such as building new hospitals and upgrading existing facilities, are essential for improving access to timely care.
- Training for Medical Personnel: Continuous training for emergency and CCU staff to handle heart attack cases efficiently can ensure that patients receive timely care. Regular drills and simulations can help staff stay prepared for real-life emergencies.
Conclusion
Reducing door-to-balloon time in India requires a multifaceted approach, focusing on patient awareness, streamlined hospital procedures, financial support, and infrastructure improvements. By addressing these areas, we can significantly improve patients’ outcomes from acute myocardial infarction. Time is indeed muscle, and every minute saved can translate to lives saved and a better quality of life post-treatment. With concerted efforts from healthcare providers, government agencies, and the community, we can ensure that heart attack patients receive the prompt and effective care they need to survive and thrive.
References
- Bhatt, D. L., & Eagle, K. A. (2018). Reducing the Door-to-Balloon Time for Patients With ST-Segment Elevation Myocardial Infarction. Circulation, 137(11), 1241–1243.
- Naidu, S. S. (2012). Clinical and Economic Burden of Recurrent Myocardial Infarction and Angina: A Review. Journal of Managed Care & Specialty Pharmacy, 18(4), S7-S13.
- Shrivastava, S. R., & Shrivastava, P. S. (2014). Improving Acute Coronary Syndrome Management in India: What More Can Be Done? International Journal of General Medicine, 7, 125–130.
- Indian Heart Association. (2023). Awareness Programs. Retrieved from Indian Heart Association.


Leave a comment